The Health Insurance Portability and Accountability Act (HIPAA) is a landmark piece of legislation enacted in 1996 to address several critical issues in the American healthcare system, including patient privacy, security of health information, and the standardization of healthcare transactions. One of the less talked about but equally important aspects of HIPAA is its impact on the medical billing process. By standardizing and regulating the way medical information is handled, HIPAA has profoundly affected how healthcare providers bill for services, how they interact with insurance companies, and how they protect patient information. This article delves into the intersection of HIPAA and the medical billing process, exploring the implications, challenges, and benefits of HIPAA compliance for healthcare providers.
1. Overview of HIPAA
HIPAA was enacted to address several critical challenges in the healthcare industry:
- Portability: Ensuring that individuals maintain health insurance coverage when changing or losing jobs.
- Accountability: Reducing healthcare fraud and abuse by establishing standards for the use and dissemination of health information.
- Administrative Simplification: Streamlining healthcare transactions by standardizing electronic data interchange, which includes the billing process.
The Act is divided into several titles, but Title II—Administrative Simplification—is particularly relevant to the medical billing process. Title II contains provisions for the standardization of electronic healthcare transactions, the establishment of national identifiers for providers, health plans, and employers, and crucially, the implementation of privacy and security regulations to safeguard patient information.
2. HIPAA and the Standardization of Medical Billing
Prior to HIPAA, the medical billing process was often cumbersome and varied significantly between providers and insurers. Differences in forms, procedures, and coding systems made it difficult to efficiently process claims, leading to errors, delays, and increased administrative costs. HIPAA addressed these issues through several key initiatives:
Standardized Code Sets: HIPAA mandated the use of standardized coding systems for diagnoses, procedures, and medical services, such as the International Classification of Diseases (ICD) codes for diagnoses and the Current Procedural Terminology (CPT) codes for procedures. This standardization allows for consistency in how medical conditions and treatments are documented, facilitating accurate billing and reducing the likelihood of errors.
Electronic Transactions Standards: HIPAA introduced standards for electronic healthcare transactions, including claims submission, eligibility inquiries, claim status requests, and remittance advice. These standards, known as the HIPAA Transactions and Code Sets Standards, ensure that all parties use a uniform format for electronic transactions, enhancing efficiency and reducing the administrative burden on healthcare providers and insurers.
National Provider Identifier (NPI): HIPAA established the NPI as a unique identifier for healthcare providers. The NPI simplifies the identification of providers in billing transactions, ensuring that claims are correctly routed and processed. This identifier is essential for preventing fraud and ensuring that only authorized providers can bill for services.
3. The Impact of HIPAA on the Medical Billing Process
HIPAA has significantly impacted the medical billing process by introducing standardization, enhancing security, and protecting patient information. These changes have had both positive and challenging implications for healthcare providers and billing professionals.
Efficiency and Accuracy: The standardization of electronic transactions and code sets has streamlined the medical billing process, making it more efficient and reducing the likelihood of errors. Healthcare providers can now submit claims electronically using standardized formats, leading to faster processing times, fewer denials, and quicker reimbursements. This efficiency is crucial for maintaining the financial health of healthcare practices and ensuring that providers are compensated promptly for their services.
Data Security and Privacy: One of the most critical aspects of HIPAA is its focus on protecting patient information. The HIPAA Privacy Rule and Security Rule establish standards for the use, disclosure, and protection of Protected Health Information (PHI). The Privacy Rule sets limits on how PHI can be used and disclosed, while the Security Rule requires covered entities to implement safeguards to protect electronic PHI (ePHI). In the context of medical billing, these rules ensure that patient information is handled securely, reducing the risk of data breaches and unauthorized access.
Challenges of Compliance: While HIPAA has brought about positive changes in the medical billing process, it has also introduced challenges. Compliance with HIPAA’s privacy and security regulations requires significant effort and resources. Healthcare providers must implement policies and procedures to safeguard patient information, conduct regular risk assessments, train staff on HIPAA requirements, and maintain documentation of compliance efforts. Failure to comply with HIPAA can result in severe penalties, including fines and legal action, making it imperative for providers to stay up-to-date with regulatory requirements.
4. HIPAA Compliance in the Medical Billing Process
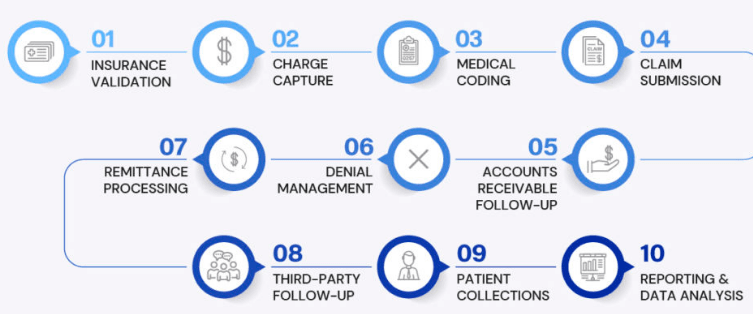
To comply with HIPAA regulations, healthcare providers and billing professionals must take several key steps throughout the medical billing process. These steps include maintaining the confidentiality of patient information, securing electronic transactions, and ensuring that billing practices align with HIPAA standards.
Confidentiality of Patient Information: Healthcare providers must ensure that patient information is kept confidential throughout the billing process. This includes implementing policies to limit access to PHI to authorized personnel only, using secure methods for transmitting and storing patient information, and obtaining patient consent for the use and disclosure of PHI for billing purposes. Additionally, providers must be cautious about sharing patient information with third-party billing companies, ensuring that these companies are also HIPAA-compliant and have signed a Business Associate Agreement (BAA).
Secure Electronic Transactions: HIPAA requires that electronic transactions involving PHI, such as claims submission and remittance advice, be conducted securely. This means using encryption and secure communication channels to protect data from unauthorized access. Healthcare providers and billing professionals must ensure that their electronic billing systems comply with HIPAA’s Security Rule, which includes implementing technical safeguards, such as access controls, audit controls, and transmission security.
Audit and Monitoring: Regular auditing and monitoring of the billing process are essential for HIPAA compliance. Healthcare providers should conduct periodic audits of their billing practices to identify potential compliance issues, such as unauthorized access to PHI or improper use of patient information. Monitoring systems should be in place to track access to electronic billing systems and detect any suspicious activity. Prompt action should be taken to address any compliance issues identified through audits and monitoring.
Training and Awareness: Ongoing training and awareness programs are crucial for ensuring that staff involved in the medical billing process understand their responsibilities under HIPAA. Training should cover key aspects of HIPAA compliance, including the proper handling of PHI, the importance of confidentiality, and the steps to take in the event of a data breach. By educating staff about HIPAA requirements, healthcare providers can reduce the risk of non-compliance and ensure that patient information is handled appropriately.
5. Benefits of HIPAA Compliance for Medical Billing
While HIPAA compliance requires effort and resources, it offers several benefits for the medical billing process, healthcare providers, and patients.
Enhanced Patient Trust: Compliance with HIPAA’s privacy and security regulations helps build trust with patients, who are increasingly concerned about the confidentiality and security of their health information. By demonstrating a commitment to protecting patient information, healthcare providers can foster a positive relationship with patients, leading to improved patient satisfaction and loyalty.
Reduced Risk of Data Breaches: HIPAA compliance reduces the risk of data breaches and unauthorized access to patient information. By implementing robust security measures, healthcare providers can protect against cyber threats and ensure that patient information remains secure. This not only safeguards patient privacy but also protects providers from the financial and reputational damage associated with data breaches.
Streamlined Billing Processes: The standardization of electronic transactions and code sets under HIPAA has streamlined the medical billing process, making it more efficient and reducing administrative burdens. Standardized billing practices lead to faster claims processing, fewer errors, and quicker reimbursements, benefiting both healthcare providers and patients.
Compliance with Legal and Regulatory Requirements: Adhering to HIPAA regulations ensures that healthcare providers are compliant with legal and regulatory requirements, reducing the risk of penalties and legal action. By maintaining HIPAA compliance, providers can operate with confidence, knowing that they are meeting their obligations to protect patient information and adhere to industry standards.
6. Future Considerations for HIPAA and Medical Billing
As the healthcare landscape continues to evolve, healthcare providers and billing professionals must remain vigilant in their efforts to comply with HIPAA and protect patient information. Several future considerations are relevant to HIPAA compliance in the medical billing process:
Technological Advancements: Advances in technology, such as the use of electronic health records (EHRs), telehealth, and mobile health applications, present new challenges and opportunities for HIPAA compliance. Healthcare providers must ensure that these technologies are secure and comply with HIPAA’s privacy and security regulations. As technology evolves, providers will need to stay updated on emerging threats and implement appropriate safeguards to protect patient information.
Increasing Cybersecurity Threats: Cybersecurity threats are a growing concern in the healthcare industry, with data breaches and ransomware attacks becoming more common. Healthcare providers must invest in robust cybersecurity measures to protect against these threats and ensure the security of electronic billing systems. Regular risk assessments, employee training, and incident response planning are essential components of a comprehensive cybersecurity strategy.
Interoperability and Data Sharing: Efforts to improve interoperability and data sharing among healthcare providers and insurers have the potential to enhance the efficiency of the medical billing process. However, increased data sharing also raises concerns about privacy and security. Healthcare providers must balance the need for interoperability with the need to protect patient information, ensuring that data sharing practices comply with HIPAA regulations.
Regulatory Changes: The regulatory environment for healthcare is continually evolving, with changes to HIPAA and other regulations potentially impacting the medical billing process. Healthcare providers must stay informed about regulatory changes and adjust their compliance efforts accordingly. By keeping abreast of regulatory developments, providers can ensure that they remain compliant and continue to protect patient information.
Conclusion
The Health Insurance Portability and Accountability Act has had a profound impact on the medical
billing process, bringing about standardization, enhancing security, and protecting patient information. While HIPAA compliance presents challenges, it offers significant benefits for healthcare providers, billing professionals, and patients. By adhering to HIPAA’s privacy and security regulations, healthcare providers can streamline their billing processes, reduce the risk of data breaches, build patient trust, and ensure compliance with legal and regulatory requirements. As the healthcare landscape continues to evolve, providers must remain vigilant in their efforts to comply with HIPAA and protect patient information, ensuring that they can continue to deliver high-quality care in a secure and efficient manner.